Alzheimer's Disease
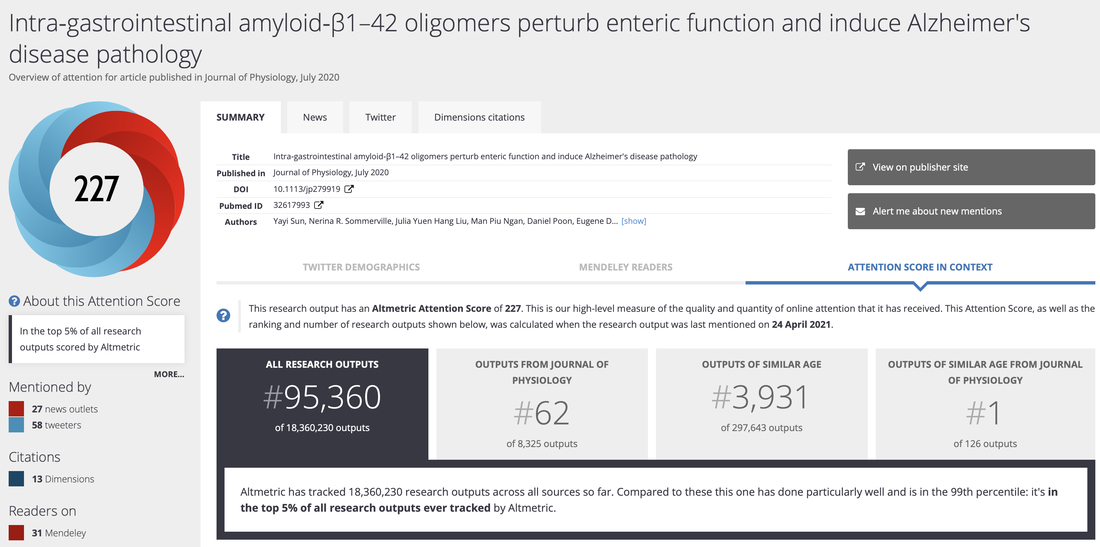
Our recent publication in the Journal of Physiology Ranks Number 1 in outputs of a similar age.
Intra-gastrointestinal amyloid-β1–42 oligomers perturb enteric function and induce Alzheimer's disease pathology
Yayi Sun, Nerina R. Sommerville, Julia Yuen Hang Liu, Man Piu Ngan, Daniel Poon, Eugene D. Ponomarev, Zengbing Lu, Jeng S. C. Kung, John A. Rudd
https://doi.org/10.1113/JP279919
Intra-gastrointestinal amyloid-β1–42 oligomers perturb enteric function and induce Alzheimer's disease pathology
Yayi Sun, Nerina R. Sommerville, Julia Yuen Hang Liu, Man Piu Ngan, Daniel Poon, Eugene D. Ponomarev, Zengbing Lu, Jeng S. C. Kung, John A. Rudd
https://doi.org/10.1113/JP279919
Alzheimer's Disease (AD) is the most common fatal neurodegenerative disorder, affecting an estimated 34 million people worldwide by the year 2025. There is currently no known cure for this devastating disease. The U S Food and Drug Administration (FDA) has approved 5 medications for the symptomatic treatment of AD and on average they are effective for 6-12 months in about half the individuals who take them.
Background
- AD is characterised by the presence of senile plaques (Beta Amyloid) and neurofibrillary tangles (Tau) that finally result in synaptic and neuronal loss.
- The 'Amyloid Hypothesis' was first proposed in the mid 80's showing that senile plaques in AD brain tissue composed primarily of the beta amyloid (AB) peptide.
- A new understanding of the amyloid cascade hypothesis proposes an alternative mechanism (soluble AB oligomers) for the initial cognitive decline.
- There is evidence of an elevated frequency of parallel involvement of the gastro-intestinal tract (GIT) and central nervous system (CNS) when neuropathology is concerned.
Beta Amyloid

- A naturally secreted small peptide (4 kDa), that results from proteolytic cleavage of the larger amyloid precursor protein (APP).
- There are 2 major AB forms, the 40 residue AB (1-40) peptide and the 42 residue AB (1-42) peptide, which differ in the absence or presence of 2 extra C-terminal residues.
- Previous research supports a physiological role for AB in normal synapse function. Increased neuronal activity enhances AB production while both APP and AB are part of a negative feedback loop controlling neuronal excitability.
- It is thought that the longer AB (1-42) is more pathogenic, due to the higher levels found within senile plaques of sporadic AD cases and even higher levels found in early-onset familial AD cases.
- While in familial forms of AB, genetic mutations result in an increased AB production or aggregation, in sporadic AD, failure of clearance mechanisms may play a central role.
Tau

- Constitutes a group of 6 isoforms involved in tubulin polymerization, microtubule stabilisation and thus axonal transport as well as cytoskeleton signalling.
- Hyperphosphorylation inhibits microtubule assembly promoting instability.
- Extracellular fibrillary tangles are mainly composed of hyperphosphorylated tau. Furthermore, alterations in tau are highly associated with the aging process in humans.
- Recently, a 'tau-axis-hypothesis' links AB and tau pathology. Increasing levels of AB trigger increased phosphorylation of tau. As a consequence tau binding to microtubules is compromised causing accumulation and neuronal toxicity.
Beta Amyloid Hypothesis
Research over the last one and a half decades, focused on the pathobiology of AD support the hypothesis which includes the following:
- A progressive cerebral accumulation of AB which initiates a complex multi-cellular cascade.
- Neuritic dystrophy
- Microgliosis
- Astrocytosis
- Neuronal dysfunction and loss
- Synaptic alterations
- Neurotransmitter deficits
- This cerebral accumulation is due to a gradual and chronic imbalance in the production vs clearance of AB.
Updating the Amyloid Hypothesis
- The hallmark of progressive deposition of insoluble fibrillar AB in senile plaques was proposed initially.
- The magnitude of fibrillar AB load correlates poorly with severity of clinical dementia challenges the original hypothesis.
- Many studies demonstrate that the best statistical correlation occurs with measures of synapse density and degree of dementia and not fibrillar AB load.
- A new understanding suggests that soluble assembly states of AB peptides are better candidates for inducing neuronal and/or synaptic dysfunction.
- These small soluble oligomers can cause cognitive decline by disrupting synaptic function in the absence of significant neuro-degeneration.
Enteric Nervous System
- The enteric nervous system (ENS) is a complex network of neurons and glia, reminiscent of the central nervous system (CNS), innervating the gut and controlling intestinal function.
- The occurrence of enteric pathology in dementia is well recognised.
- Gastro-intestinal dysfunction, particularly constipation (a clinical expression of enteric neurodegeneration), is a prevalent symptom in neurologic and systemic diseases associated with neurodegeneration. This dysfunction is partly related to abnormalities and cell loss in the ENS.
- Additionally, during aging there is evidence of a loss of excitatory (cholinergic) enteric neurons and interstitial cells of Cajal whereas inhibitory neurons appear unaffected.
- A cholinergic hypothesis of neuronal vulnerability in the CNS is thought to contribute to the cognitive decline seen in aging and neurodegenerative disease.
- Beta amyloid (AB) peptides and it's precursors are well described in the peripheral nervous system including the ENS.
- Recently, a transgenic AD mouse model confirmed the presence of AB in the small and large intestine during aging.
- The ENS may provide a valuable entity to study the pathophysiology of neurodegeneration as well as present as a pathological marker during early stages of AD.
A Working Hypothesis

- The enteric nervous system (ENS) may be a gateway for the pathological process which occur in the GIT first and later spread to the CNS.
- Recently, a transgenic AD mouse model confirmed the presence of AB in the small and large intestine during aging.
- The amyloid forms involved in AD are reported to be 'prion-like' and may follow similar mechanisms of cell to cell spread.
- Normal prion protein (PrPc), expressed in both human and animal ENS can function as a cell surface receptor for toxic AB oligomers.
Prion Protein
The normal prion protein isoform (PrPc) is a naturally occurring cellular protein expressed in all tissue of the human body with highest levels expressed in the central nervous system (CNS). Functions include:
An abnormal isoform PrPsc is capable of inducing prion diseases such as Transmissible Spongiform Encephalopathies (TSEs). After initial infection and prion replication, prions migrate from the peripheral regions of the host to the CNS, culminating in a fatal neurodegenerative process.
More commonly, the peripheral entry point for PrPsc is the gastro-intestinal tract (GIT). Haematopoietic cells, lymphoid cells and secondary lymphoid organs play a critical role to facilitate initial site of replication and transport to the CNS via sympathetic (Splanchic) or parasympathetic (Vagus) fibres of the enteric nervous system (ENS).
Involved in this process are exosomes, small membranous vesicles secreted by a number of cells including neurons. Ultimately they play an important role in cell to cell spread, removal of unwanted protein and transfer of pathogens between cells.
- Immunoregulation
- Signal transduction
- Synaptic transmission
- Protect against or induce apoptosis
An abnormal isoform PrPsc is capable of inducing prion diseases such as Transmissible Spongiform Encephalopathies (TSEs). After initial infection and prion replication, prions migrate from the peripheral regions of the host to the CNS, culminating in a fatal neurodegenerative process.
More commonly, the peripheral entry point for PrPsc is the gastro-intestinal tract (GIT). Haematopoietic cells, lymphoid cells and secondary lymphoid organs play a critical role to facilitate initial site of replication and transport to the CNS via sympathetic (Splanchic) or parasympathetic (Vagus) fibres of the enteric nervous system (ENS).
Involved in this process are exosomes, small membranous vesicles secreted by a number of cells including neurons. Ultimately they play an important role in cell to cell spread, removal of unwanted protein and transfer of pathogens between cells.
Therapeutic Implications
It has been hypothesized that the GIT may represent an entry point for altered proteins, such has been demonstrated in prion diseases and now postulated for other neurodegenerative diseases such as AD.
The hypothesis of transmissibility of ND's could alter future therapeutic approaches. Combining cell substitution therapy (stem cells) with treatments that block cell to cell spread could aid in limiting the recruitment of stem cells in the spread of neurodegeneration. Furthermore, such novel treatments may limit the actual spread of misfolded proteins especially during early stages of the disease prior to permanent pathological changes. |
Involvement in Neurodegenerative Diseases (ND's)
- PrPc can function as a cell surface receptor for toxic beta amyloid (AB) oligomers and this interaction seems to be critical for AB-oligomer mediated disruption of synaptic function.
- Exosomes are involved in the processing of amyloid precursor protein (APP) which is associated with Alzheimer's Disease (AD). Exosomes have been shown to contain full length APP and its cleaved products including AB.
- Exosomes may provide a means of intracellular to extracellular transport of such proteins during the pathogenesis of AD as well as cell to cell spread.
- Exosomal markers have been shown to be enriched in amyloid plaques in the brains of mice and post mortem samples of human AD patients. This again indicates that the trafficking of AB aggregates during disease progression may partly rely on similar transport mechanisms seen in prion diseases.
In Summary

The presence of beta amyloid in the gastro-intestinal tract with the possibility of spread to the CNS using 'prion-like' mechanisms via peripheral nerves or the blood constitute an interesting hypothesis. As well as the gastro-intestinal tract having the capacity to be a pathological marker for neurodegeneration , the enteric nervous system may be an invaluable site for studying the pathophysiology of neurodegeneration in both aging and AD.
References
Aguzzi, A., et al. (2006). ''Pathogenesis of prion diseases: current status and future outlook.'' Nat Rev Microbiol 4(10): 765-775.
Bellingham, S.A., et al. (2012). ''Exosomes: vehicles for the transfer of toxic proteins associated with neurodegenerative diseases?'' Front Physiol 3(124): 1-12.
Camilleri, M., et al. (2008). ''Enteric neurodegeneration in ageing.'' Neurogastroenterol Motil 20(3): 185-196.
Cushman, M., et al (2010). ''Prion-like disorders: blurring the divide between transmissibility and infectivity.'' J Cell Sci 123(8): 1191-1201.
Hou, L., et al (2004). ''Solution NMR studies of the AB (1-40) and AB (1-42) peptides establish that the met35 oxidation state effects the mechanism of amyloid formation.'' J. Am. Chem. Soc. 126(7): 1992-2005.
Marcello, E., et al (2012). ''Synaptic dysfunction in Alzheimer's disease.'' Adv Exp Med Biol 970: 573-601.
Natale, G., et al. (2011). ''Parallel manifestations of neuropathologies in the enteric and central nervous systems.'' Neurogastroenterol Motil 23(12): 1056-1065.
Pallas, M., et al. (2008). ''From aging to Alzheimer's disease: Unveiling ''the switch'' with the senescence-accelerated mouse model (SAMP8).'' J Alzheimers Dis 15(4): 615-624.
Selkoe, D.J. (2001). ''Alzheimer's disease results from the cerebral accumulation and cytotoxicity of amyloid B protein.'' J Alzheimers Dis 3(1): 75-80.
Zussy, C., et al (2013). ''Alzheimer's disease related markers, cellular toxicity and behavioural deficits induced six weeks after oligomeric amyloid-B peptide injection in rats.'' PLOS ONE 8(1): 1-19.
Alzheimer's Association. (2013) Science & Progress, Current Alzheimer's Treatments [online] Available from www.alz.org [accessed 25 February 2013].
Bellingham, S.A., et al. (2012). ''Exosomes: vehicles for the transfer of toxic proteins associated with neurodegenerative diseases?'' Front Physiol 3(124): 1-12.
Camilleri, M., et al. (2008). ''Enteric neurodegeneration in ageing.'' Neurogastroenterol Motil 20(3): 185-196.
Cushman, M., et al (2010). ''Prion-like disorders: blurring the divide between transmissibility and infectivity.'' J Cell Sci 123(8): 1191-1201.
Hou, L., et al (2004). ''Solution NMR studies of the AB (1-40) and AB (1-42) peptides establish that the met35 oxidation state effects the mechanism of amyloid formation.'' J. Am. Chem. Soc. 126(7): 1992-2005.
Marcello, E., et al (2012). ''Synaptic dysfunction in Alzheimer's disease.'' Adv Exp Med Biol 970: 573-601.
Natale, G., et al. (2011). ''Parallel manifestations of neuropathologies in the enteric and central nervous systems.'' Neurogastroenterol Motil 23(12): 1056-1065.
Pallas, M., et al. (2008). ''From aging to Alzheimer's disease: Unveiling ''the switch'' with the senescence-accelerated mouse model (SAMP8).'' J Alzheimers Dis 15(4): 615-624.
Selkoe, D.J. (2001). ''Alzheimer's disease results from the cerebral accumulation and cytotoxicity of amyloid B protein.'' J Alzheimers Dis 3(1): 75-80.
Zussy, C., et al (2013). ''Alzheimer's disease related markers, cellular toxicity and behavioural deficits induced six weeks after oligomeric amyloid-B peptide injection in rats.'' PLOS ONE 8(1): 1-19.
Alzheimer's Association. (2013) Science & Progress, Current Alzheimer's Treatments [online] Available from www.alz.org [accessed 25 February 2013].